

These terms have been replaced by the term “myofascial pain.”įor many clinicians and investigators, the finding of one or more myofascial trigger points (MTrPs) is required to assure the diagnosis of MPS. 3, 4 Nomenclature from the past included “fibrositis” which implied inflammation of the connective tissue lining muscle, along with chronic muscle pain. The term “myofascial” has evolved from the view that both muscle and fascia are likely to be contributors to the symptoms. This heralds the sensitized state, one of the features of a chronic pain disorder, in which the pain itself is the pathology and requires medical intervention for its resolution. In some cases, however, muscle pain persists long after resolution of the injury it may even refer to other parts of the body, usually contiguous or adjacent rather than remote. This type of pain frequently resolves in a few weeks with or without medical treatment. Few people live without ever having experienced muscle pain as a result of trauma, injury, overuse, or strain. Myofascial pain is prevalent and a frequent cause of visits to primary care physicians and pain clinics 1, 2. The criteria for diagnosis and their relative importance have evolved over time. Myofascial pain is a clinical problem that has generated interest and confusion for decades. The authors will chronicle the advances that have led to the current understanding of MTrP pathophysiology and its relationship to MPS, and review the contributions of clinicians and researchers who have influenced and expanded our contemporary level of clinical knowledge and practice.
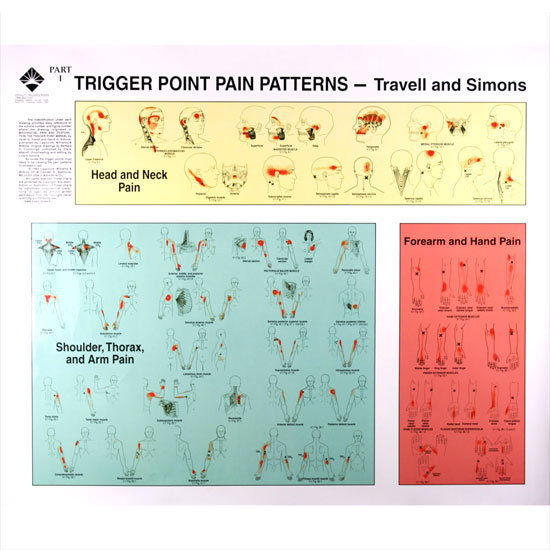
Data suggest that the soft tissue milieu around the MTrP, neurogenic inflammation, sensitization, and limbic system dysfunction may all play a role in the initiation, amplification, and perpetuation of MPS. In order to address these deficiencies, investigators have recently applied clinical, imaging (of skeletal muscle and brain), and biochemical analyses to systematically and objectively study the MTrP and its role in MPS. Unfortunately, much of the terminology, theories, concepts, and diagnostic criteria are inconsistent, incomplete, or controversial. According to Travell and Simons, MTrPs are central to the syndrome-but are they necessary? Although the clinical study of muscle pain and MTrPs has proliferated over the past two centuries, the scientific literature often seems disjointed and confusing. MPS is a term used to describe a pain condition which can be acute or, more commonly, chronic and involves the muscle and its surrounding connective tissue (e.g.
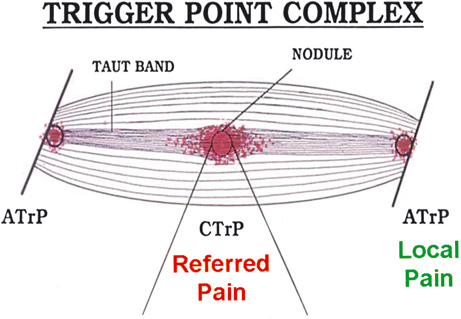
active), or painful only on compression (i.e. MTrPs are hard, discrete, palpable nodules in a taut band of skeletal muscle that may be spontaneously painful (i.e. The intent of this paper is to discuss the evolving role of the myofascial trigger point (MTrP) in myofascial pain syndrome (MPS) from both a historical and scientific perspective.


 0 kommentar(er)
0 kommentar(er)
